Blood test detects susceptibility to aggressive rectal cancer
Research shows that patients’ immune systems are activated to varying degrees by normal chemotherapy.
More Norwegian men and women are now being diagnosed with rectal cancer than previously, and the prevalence of the disease in Norway is among the highest in the world, according to the Cancer Registry of Norway. Every year 1300 Norwegians get rectal cancer, compared with only 266 cases per year in the 1950s.
These findings correlate with a study led by American Cancer Society researchers, which reveals that incidence rates for colon cancer and rectal cancer have been increasing for adults under age 50 since the mid-2000s.
Norway has seen a fivefold increase in rectal cancer in recent decades.
Researchers have been working intensely to make treatment more effective. New discoveries offer hope that more lives can be saved by individualizing patient treatment.
Course of disease varies
Rectal cancer can run a completely different course from one patient to the next, even when the cancer has reached the same stage and patients have received the same treatment. The disease spreads faster in some patients and is then harder to treat.
Sebastian Meltzer is a rectal cancer researcher who recently defended his PhD dissertation on the subject in the University of Oslo ‘s Institute of Clinical Medicine.
"My findings suggest that some patients’ immune systems may not activate as well as others," Meltzer said.
He tested the blood of patients who received standard treatment and patients who received intensive treatment in the form of chemotherapy prior to radiation therapy and surgery.
He discovered differences in both patient groups that may be beneficial for future treatment.
Disease has often spread when cancer is detected
In some patients rectal cancer is diagnosed as a small tumour. In other patients the disease has already spread to other organs, or metastasized, by the time it’s diagnosed.
"The cancer often spreads to the liver or lungs in people who have early metastasis, but it may also spread to other organs in the pelvis, abdomen, lungs or skeletal system. The prognosis is far worse in these cases,” says Meltzer.
So why can’t the cancer be detected earlier? Meltzer says there may be several reasons. “Either the tumour is particularly aggressive and has managed to spread by the time symptoms are noticed, or it’s grown slowly with no symptoms and has already spread when the patient is diagnosed,” he says.
Varied responses to chemotherapy and radiation
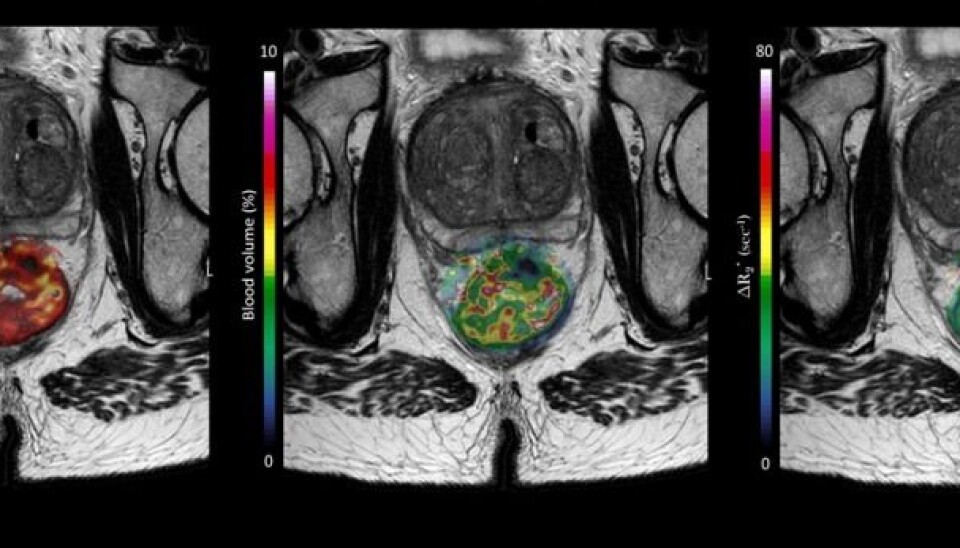
Patients who have a rectal tumour that has grown through the intestinal wall or into other pelvic organs at the time of diagnosis are typically offered targeted radiation therapy along with chemotherapy prior to surgery.
Most people respond well to this treatment. But for a few, it doesn’t achieve the desired effect. While many patients remained cancer-free after five years of follow-up care, other patients quickly relapsed.
"I wanted to figure out why patients responded so differently to the treatment, and whether we could determine who’s more vulnerable from the start," says Meltzer.
Differences in blood samples
Meltzer took blood samples of patients diagnosed with rectal cancer before, during and after treatment.
His study included patients both with and without metastasis when the diagnosis was made.
He found that already at an early stage in the disease, the amount of two specific proteins in the blood was different between these two groups.
"These are substances that can give a picture of the aggressiveness of the disease and treatment response," says Meltzer.
The two proteins are connected to the production of immune cells, which in turn is an expression of how well or poorly the patient's own immune system will be activated by the treatment, he explains.
Some people see a big increase of these proteins during treatment while others see very little increase.
"What we think is happening during the pre-treatment is that the immune system is able to mobilize quickly in some patients, and this is reflected in an increase of these proteins in the blood. They have a kind of acute immune response to the cancer,” says Meltzer.
For these patients, an additional blood test can provide insight into the biology of the disease, and enable the treatment to be adapted to the individual patient.
Chronic inflammation
Meltzer found differences in these protein levels from the start.
"This means that even before you start treatment, you can see who’ll benefit from the treatment and who won’t," he says.
Patients who have a lot of these particular proteins in the blood before treatment begins may have a form of treatment resistance. Meltzer also found that these patients have symptoms that may resemble chronic inflammation, resulting from the tumour.
"This means that the body can’t respond to the treatment," he says.
Meltzer hopes that his research findings can be used to provide patients who show signs of chronic inflammation with a different, and perhaps more intensive, pre-treatment.
"Maybe they need more or different treatment to boost their immune system," Meltzer says.
Decrease in the elderly, increase among younger adults
The incidence of colon cancer in Norway is high, with Norwegian women ranking at the top of the list worldwide in 2012.
Meltzer says improved screening has likely contributed to new numbers that suggest rectal cancer is decreasing in the traditional older age groups. At the same time, increases are occurring in both younger people and overall because the population is getting older, resulting in a net increase.
And even though rectal cancer is easier to detect, it is often more aggressive than colon cancer.
The increase in rectal cancer among young adults “may have something to do with diet, but also with less physical activity,” says Meltzer. “Smoking used to be an important risk factor. Research is suggesting that a lack of vitamin D and changes in intestinal bacteria may also be factors,” he says.
Testing immunotherapy
Meltzer is about to embark on a new research project to try to improve the prognosis for people with rectal cancer.
He describes the new study, called METIMMOX: “We’re going to combine traditional chemotherapy and immunotherapy for patients with colorectal cancer that has metastasized.”
Meltzer will then analyze blood samples from the patients who receive this combination treatment and compare them with a control group. The Kolbjørn Brambani Fund has awarded him a research grant to be used for the project analyses. All the university hospitals in Norway are participating in the project, which is scheduled to start in March 2018.
Reference:
Sebastian Meltzer: Circulation Markers of Immunogenicity and Metastasis in Combined-Modality Treatment of Rectal Cancer. Doctoral thesis defence 14 December 2017, Akershus University Hospital.
-------------------------------------






























