If the placenta is too large or
too small, something may be wrong.
But measuring it is far from simple.
A new way of measuring the placenta aims to detect pregnancies at risk
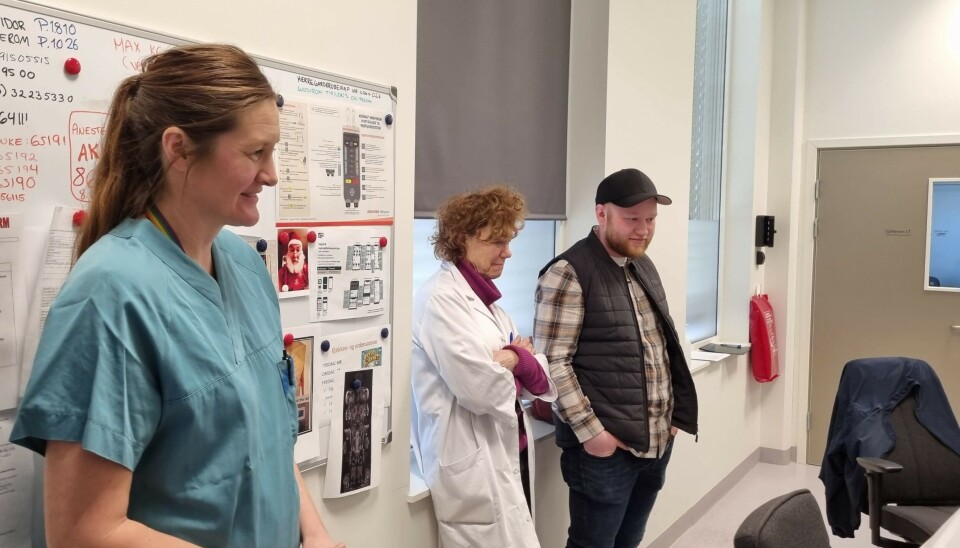
Ahus Hospital Gardermoen, a Saturday afternoon in March.
Five people have gathered in a small back room. They are all staring at the same screen.
What looks like an oversized, light grey aubergine changes shape as the radiologist adjusts the settings on the computer.
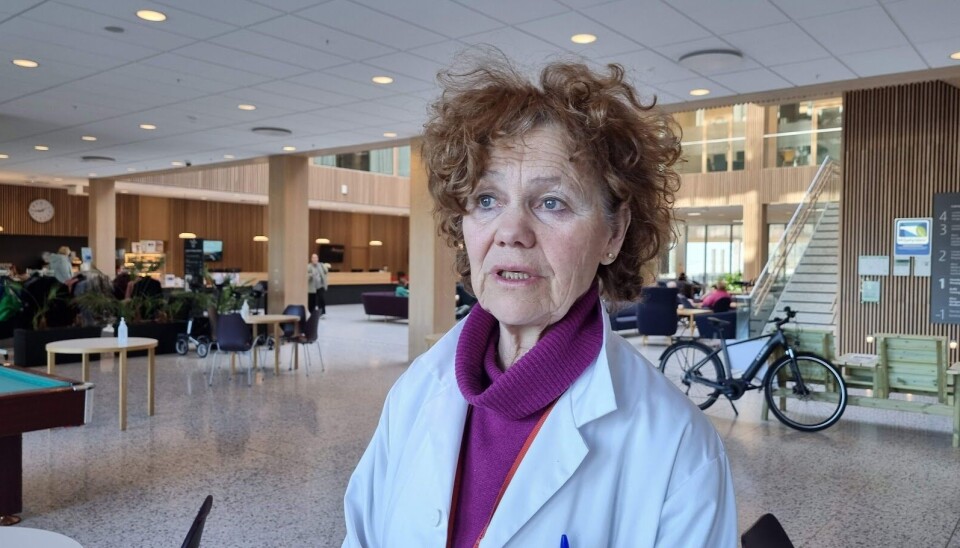
"Now you can see how big the organ is," researcher Anne Eskild tells the young man in a cap and puffer vest while pointing at the screen.
Erlend Holten is about to become a father for the first time.
On the other side of the wall, his girlfriend Karoline Haugsjordet is lying inside a large scanner.
Rhythmic swooshing and pumping sounds from the MRI machine reach the back room.
But the couple is not here to check on how the baby is doing.
They are participating in a research project about the organ we all depended on for nine months. The placenta.
Dramatic events
This short-lived organ can in fact sound the alarm if something is wrong.
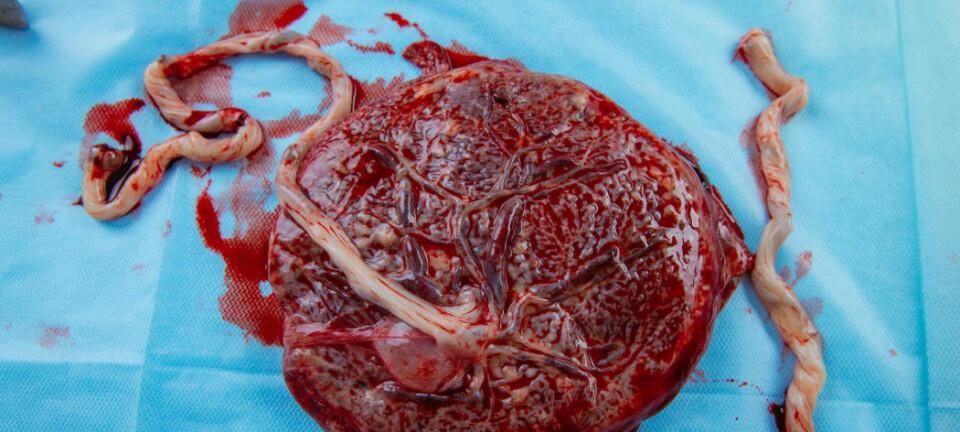
After birth, the placenta comes out. It is weighed and recorded. Then it is thrown in the bin.
Using information from the Medical Birth Registry of Norway, researchers have uncovered a pattern.
Some babies have a placenta that is either small or large compared to the baby's own size. And these children were more likely to experience dramatic events.
Most of them turned out fine. But as a group, they had a slightly higher risk of dying in the womb or shortly after birth. They were also more likely to develop cerebral palsy, which is caused by a brain injury.
Eskild was the project leader for these studies.

In recent years, Eskild and her colleagues at Ahus Hospital have had a new goal in mind.
To use their knowledge to help mother and child.
" Maybe during pregnancy, we can identify cases where there’s an imbalance between the placenta and the baby. That way, in the long term, we might be able to prevent foetal death," says Eskild.
The idea was simple.
Since ultrasound is the standard method for examining the foetus, wouldn't it make sense to measure the placenta at the same time, when pregnant women come in for a check-up?
"That's exactly what we thought. This must be a piece of cake," she says.
A new type of ultrasound
It turned out to be far from the truth.
The MRI images the researchers took of the placenta did not match the ultrasound measurements.
The researchers were puzzled. MRI is so precise that it can be used as a gold standard. But such an expensive and labour-intensive method can't be used on all pregnant women.
Then one day, while Eskild was skiing with a friend, she heard about a new type of ultrasound.
It had been developed at SINTEF Digital to examine the brain.
Infrared tracking and artificial intelligence
In a new room, Karoline has lain down on a bench with her jumper pulled up. Her belly is covered in sticky gel.
"We would prefer not to know the sex," she says to the three researchers in the room.
Karianne Sagberg, a doctor and researcher at Ahus Hospital, assures the couple that the examination will not reveal anything.
"But it's in the DNA of the placenta," she adds.

The placenta, which functions as a strictly guarded checkpoint between mother and child, actually originates from the baby's own cells.
For months, it takes over the role of several of the baby's organs – such as the lungs, kidneys, and intestines.
"Are you ready?" asks the third researcher.
Torgrim Lie has brought equipment from SINTEF Digital this weekend.
Now he's sitting behind a laptop at a small table in the corner of the room.

"Yes," answers the other doctor in the room, Helene Fjeldvik Peterson.
The Ahus researcher glides a handheld probe back and forth through the gel on Karoline's stomach.
Four small reflective balls are attached to the probe.
At the head of the examination bench stands a camera with infrared light.
When the light hits the balls, the ultrasound machine can measure exactly where on the stomach the image comes from.

The measurements will be used to train artificial intelligence (AI).
"We're going to try to teach the machine to do the job for us," Sagberg explains to the expectant parents.
The goal is for AI to learn how to identify the placenta in ultrasound images – and calculate its size.

Too imprecise, says researcher
The first study of the method has already been published in the journal Minimally Invasive Therapy & Allied Technologies.
When the researchers compared the result with the MRI gold standard on 15 placentas, they got closer than before.
"I find the project to be an interesting step forward in methodology, and any research on the placenta could prove valuable in the future," says Anne Cathrine Staff.
She also conducts research on the placenta at Oslo University Hospital.
But for now, this is too imprecise to be used in clinics, Staff points out.
"The question is whether you can specify the volume precisely for every placenta," she says.
Must be linked to other indicators
Even if ultrasound in the future can measure the size with complete accuracy, that alone is not enough.
Most viewed
It still needs to be proven that such measurements actually help more foetuses make it safely through pregnancy, Staff points out.
A placenta that is too small or too large is not necessarily dangerous.
"My advice is that this method should be linked to how the placenta functions and to the outcome for the foetus," says Staff.
There are already several indicators today that can signal a poorly functioning placenta.
For example, poor blood flow from the placenta to the foetus. Or certain proteins from the placenta that end up in the mother's blood.
Have only just begun
In a break room at Ahus Hospital, the researchers have taken a coffee break.
They agree that the method still has a way to go.
"If we're going to use it in the clinic, we need a tool that's precise," says Eskild.
But they have only just begun.
Just this weekend, 40 pregnant women are being examined. With each one, the AI will hopefully get smarter.

SINTEF researcher Torgrim Lie admits that the placenta presents major challenges.
He himself is more used to imaging the brain.
"What's special about the brain is that it stays more or less fixed inside the skull. But here, nothing stays still," says Lie.
The baby often blocks the view of the placenta. And suddenly it kicks both the placenta and the handheld probe, explains Peterson.
On top of that, the organ can take on all kinds of shapes, says Eskild.
"They can be long and flat, thick and rounded, big or small," she says.
Ambitious goals
Still, they believe in the method.
"What we hope to end up with is regular ultrasound, the kind available in all prenatal clinics," says Sagberg.
In other words, without reflectors and infrared light.
What should remain is just smart software inside the ultrasound machine – software that understands how big the placenta is.
If they succeed, the first step will be to conduct more research on the placenta while the mother is pregnant.
That would allow them to study many more pregnant women.
This way, they can research how the size of the placenta inside the womb affects the health of both mother and child.
An even more ambitious goal is to commercialise the method. In that case, it could become part of a standard pregnancy check-up.
And hopefully save lives.
Placenta on stage
But the volunteers who showed up this weekend in March won't benefit from the research themselves.
Still, they might spare the placenta a bit more thought than most of us do in a lifetime.
From the stage at Eldorado cinema, on a September day in 2024, Helene Peterson also made sure the audience at the Researcher Grand Prix competition devoted ten minutes to the topic.
Holding a real placenta in her hands, she convinced both the judges and the audience that she was the best at communicating her research.

Now she's back to her daily routine. She gets up to follow Sagberg and Lie out the door.
They're off to examine the next pregnant woman on the list.
"Maybe we should all think a bit more about the placenta?"
"I don't know if it helps much for anyone other than obstetricians to think about it, but we should definitely appreciate it. Because it does a very important job," says Peterson.
The placenta shown in the gif at the top of the article came from an uncomplicated birth. It has nothing to do with either Karoline Haugsjordet or the research project at Ahus Hospital.
———
Translated by Alette Bjordal Gjellesvik
Read the Norwegian version of this article on forskning.no
References:
Dypvik et al. Placental Weight and Risk of Neonatal Death, JAMA Pediatrics, 2020. DOI: 10.1001/jamapediatrics.2019.4556
Haavaldsen et al. Fetal death and placental weight/birthweight ratio: a population study, Acta Obstetric Gynecolog Scandinavia, vol. 92, 2013. DOI: 10.1111/aogs.12105
Peterson et al. Placental size at gestational week 36: Comparisons between ongoing pregnancies and deliveries, Acta Obstetricia et Gynecologica Scandinavica, vol. 103, 2023. DOI: 10.1111/aogs.14700.
Sagberg et al. A new method for placental volume measurements using tracked 2D ultrasound and automatic image segmentation, Minimally Invasive Therapy & Allied Technologies, 2025. DOI: 10.1080/13645706.2025.2449699
Strand et al. Association of placental weight with cerebral palsy: population-based cohort study in Norway, BJOG, vol. 123, 2015. DOI: 10.1111/1471-0528.13827
Gifs: Eldrid Borgan
Emojis: OpenMoji, CC BY-SA 4.0
Related content:
Subscribe to our newsletter
The latest news from Science Norway, sent twice a week and completely free.