
Navigating menopause in the workplace:
"We can't compare the sickness absence rates of men and women"
Menopause can significantly affect a woman’s ability to work.
All women go through menopause.
For some, the challenges become so overwhelming that they can no longer continue working, often at the height of their careers.
At Arendalsuka, an annual political event in Norway, several seminars addressed the relationship between menopause and work.
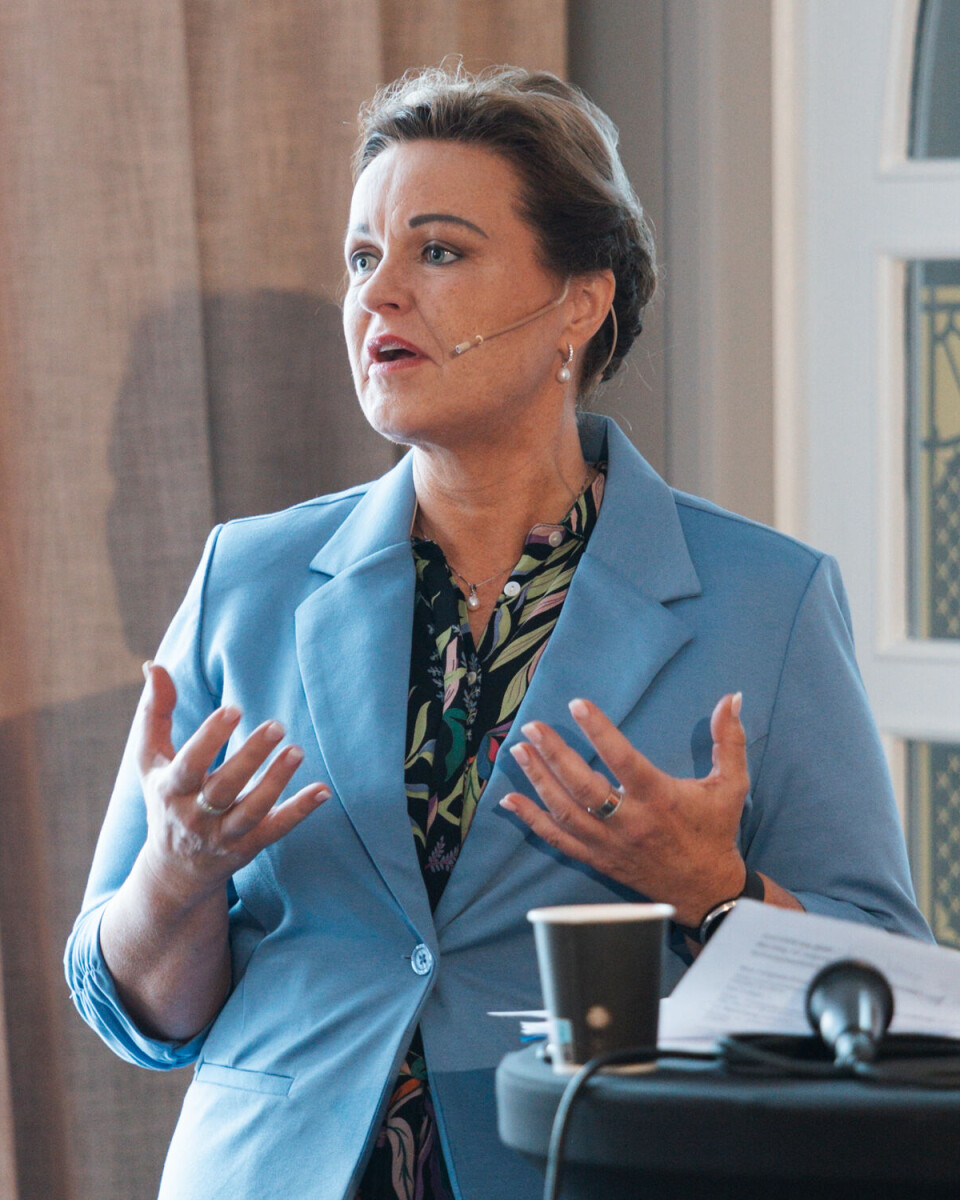
“Menopause shouldn’t be something we only whisper about at work,” says Marianne Natvik, a general medicine specialist and researcher at the University of Oslo.
How does it impact work?
“Women probably don't appreciate being called into the boss’ office to discuss their menstruation and hot flashes,” says Helena Enger.
She is a gynaecologist at Volvat, and took part in the discussions during Arendalsuka.
“However, they do want their workplace to be prepared for menopause,” she says.
This preparation might include providing information on what menopause is, available treatment options, allowing for individual accommodations, and ensuring access to a company doctor, according to Enger.
Flexible working hours should also be an option.
“If you've had a rough night, you could start work a little later. Or you could work from home if it's really bad,” says Enger.
“We can’t afford to lose resourceful women, who are often in leadership positions at this age.”
She believes that keeping menopausal women in work could save the state significant amounts of money.
GPs are not skilled enough
One of the issues raised in Arendal was whether Norwegian GPs are adequately equipped to identify the symptoms of menopause.
“Many GPs are very competent, and women themselves are very good at identifying their symptoms. But that’s only if hot flashes are the first symptom,” says Marianne Natvik. “Menopause is much more than just hot flashes.”
The challenge arises when symptoms are less clear, such as psychological issues, sleep problems, and fatigue.
“Figuring out whether these symptoms are due to menopause can be difficult, both for the GP and the woman herself,” Natvik summarises.
“We have high expectations for life, and this can lead to symptoms that mimic menopause. Additionally, this is an age when health issues may arise. So, what is ageing, and what can we really expect from our bodies?” Natvik asks.
Hormonal contraception
Natvik mentions that many women use hormonal contraception today, which means they do not have regular periods. This makes it harder to detect when menstruation stops permanently.
“We as GPs certainly have room for improvement in this area,” she admits.
Natvik also notes that more women are coming to her with menopause symptoms today compared to five years ago.

“That’s a very positive development,” she says.
Women have higher sick leave rates than men
Women have higher sick leave rates than men. This has puzzled researchers for some time, and the exact cause of these differences remains unclear. Could menopause be part of the explanation?
“We’ve stopped comparing the sickness absence of women and men,” says Inger Haukenes, a researcher at NORCE and the University of Bergen. “But I will do so in this context because it’s important.”
For men, sick leave tends to increase steadily with age, she explains.
The same is true for women, but they also have two additional peaks. One occurs during pregnancy and childbirth, and the other during menopause.
“When you look at the broader picture, it becomes evident that women’s lives include specific transitions that bring health challenges, naturally leading to higher absenteeism than men,” says Haukenes.
We should not make direct comparisons
Nevertheless, women have higher sick leave rates across all age groups.
“We should never expect that men and women will have identical rates of absenteeism. That would be unrealistic and unfair to women. We need to recognise that these differences are significant and understand that this is the reality. We must stop making direct comparisons,” the researcher says.

Haukenes mentions that she and her colleagues at the University of Bergen have spent years investigating the reasons behind gender differences in sick leave.
“There are many theories, but I don't think we’ll ever fully understand it. It’s not relevant, nor is it important, to compare sickness absence rates between men and women,” she says.
Have we truly considered all the options?
Not every profession allows for flexible hours or the possibility of working from home. This is especially true for roles in childcare, education, healthcare, and other jobs requiring shift work.
But are we really so sure about that? Wonders Nina Tangnæs Grønvold. She leads the public committee focused on women's health and work – the Women’s Occupational Health Committee.
“We’ve grown accustomed to the idea that many employees have jobs where flexibility is almost impossible. These are roles where people depend on your constant presence,” says Grønvold.
However, she suggests that perhaps we haven’t fully explored the possibilities within these sectors.
“If the workplace had been shaped by more women, or if it were designed in 2024 instead of 100 years ago, it might look a little different,” she says. “This also ties into the availability of other workers and resources.”
A language for menopause
Most of the attendees at Arendal agreed that we need to improve how we talk about menopause.
How can women experiencing menopause and their managers discuss it without it being awkward, too personal, or challenging?
“We need a language that both women and men can use comfortably, without resorting to giggles, jokes, or dark humour. Many still feel the need to joke or make light of these topics when discussing them,” says Grønvold.
“Many managers in the public sector aren’t necessarily inclined to joke or make light of this issue in a one-on-one setting with an employee. We need a more serious approach, both in how we talk about and address these matters,” she says.
She also highlights the importance of finding a way to discuss other topics, like pregnancy, breastfeeding, endometriosis, menstruation, abortion, and assisted reproduction, alongside menopause.
“It feels very unnatural for these conversations to be limited to women alone,” says GP Marianne Natvik.
———
Translated by Alette Bjordal Gjellesvik
Read the Norwegian version of this article on forskning.no






































